
Mayo Clinic John E. Herman Home and Treatment Facility
The Mayo Clinic John E. Herman Home and Treatment Facility is a residential treatment program for adults who have a serious mental illness. Its goal is to help residents return to the community to engage in value-driven, productive and meaningful lives.
People in the program experience:
• Individualized treatment of psychiatric symptoms
• On-site, 24/7 support from a multidisciplinary team
• A supervised environment
• A stay of at least three months, usually
• Evidence-based individual and group therapy
• An opportunity to gain competitive employment in the community through an evidence-based vocational program, individual placement and support (IPS)
• Dedicated time for activities of daily living, physical activity and recreation, facility maintenance, and leisure
People age 18 or up may be eligible for the program if they are living with mood disorders (such as depression and bipolar disorder), psychotic disorders (such as schizophrenia), anxiety or personality disorders.
The program includes a treatment facility and two residential recovery homes in Rochester, Minnesota. The homes each have eight rooms with private baths and communal spaces for cooking and gathering.
Self-referrals are considered, as are referrals by family members and providers.
Mayo Clinic Psychiatric Hospital
In the hospital, psychiatrists work in integrated teams with internists, psychologists, social workers, physical and occupational therapists, and other specialists to provide comprehensive coordinated short-term care tailored to the needs of each patient. The hospital includes these units:
• Psychiatric Acute Care Unit. This unit stabilizes and treats adults experiencing mental health crises, such as those who are suicidal, homicidal or psychotic. After being stabilized and evaluated, patients receive individualized care, which may include medical treatments, group psychotherapy, recreational therapy, and education about coping strategies, relapse prevention, and stress management.
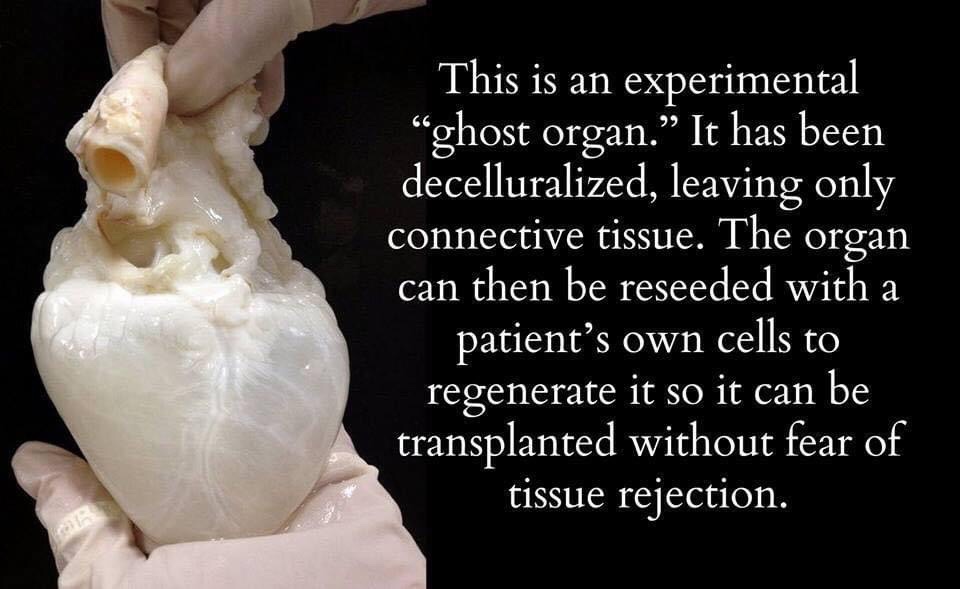
• Medical and Geriatric Psychiatry Unit. Admitted to this unit are adults with both medical and psychiatric conditions, as well as geriatric patients who need hospitalization for psychiatric issues — most commonly late-life mood and cognitive disorders. Treatment may include medication, recreational and relaxation therapy, and education about depression, anxiety and aging-related issues.
• Mood Disorders Unit. This unit treats adults whose depression or bipolar illness is significantly affecting their quality of life, functioning or safety. Intensive daily treatment is personalized to each patient and may include talk therapy (psychotherapy), such as cognitive behavioral therapy, dialectical behavioral therapy, acceptance and commitment therapy or behavioral activation. Treatment may also involve medications, family and group therapy, occupational therapy, relaxation activities, and — when appropriate — electroconvulsive therapy (ECT) or transcranial magnetic stimulation (TMS).
• Child, Adolescent and Family Services Unit: This secure unit specializes in stabilization and treatment for children and teenagers who are experiencing an acute mental health crisis, such as those who are suicidal, homicidal or experiencing psychosis. Treatment for a variety of conditions including mood and adjustment disorders, anxiety, self-injurious behavior and psychotic disorders is family-centered and multidisciplinary. The treatment team includes psychiatrists, advanced practice providers, psychologists, social workers, specialized nursing staff, Child Life Specialists, and occupational, physical, recreational and music therapists.
Mayo Clinic Depression Center
A member of the National Network of Depression Centers, Mayo Clinic Depression Center offers comprehensive evidence-based evaluation and treatment for adults and children with depression or bipolar disorder. Programs range from outpatient consultations to intensive inpatient treatment, with care provided by a team of Mayo Clinic psychiatrists, psychologists, nurse practitioners, social workers and other specialists with expertise in mood disorders. Services include:
• Adult Mood Clinic. Outpatient evaluation and treatment for adults with treatment-resistant depression or bipolar disorder is available in the Mayo Mood Clinic. After an initial assessment and depending on the person’s needs, he or she may be referred to the Mood Disorders Unit or the two-week Mood Program.
• Adult Mood Program. This is a 10-day, full-day group-based outpatient multidisciplinary psychotherapy for adults with depression or bipolar disorder. It uses three evidence-based supported psychotherapies: interpersonal and social rhythm therapy (also called IPSRT), mindfulness-based cognitive therapy, and behavioral activation. The program helps to develop more effective ways to manage interpersonal problems and stabilize the daily routine of activities.
• Adult Mood Disorders Unit. This inpatient unit, described above, is part of the Mayo Clinic Psychiatric Hospital, which provides expert care tailored to individual needs.
• Pediatric Mood Clinic. Staffed by experts in childhood mood disorders such as depression, bipolar disease, cyclothymic disorder and persistent depressive disorder (dysthymia), the clinic provides team-based diagnosis and treatment. Outpatient options include: Adolescents Coping with Depression, a 12-week intervention meeting for one hour a week for teens ages 14 through 18; and Multifamily Psychoeducational Psychotherapy, an 8-week intervention meeting for one hour a week for youths ages 11 through 14.
• CAIMP. The Child and Adolescent Integrated Mood Program (CAIMP) is a two-week outpatient partial hospitalization program for children and teens (ages 10 to 18) with primary depression or bipolar disorder. It’s held Monday through Friday, 8 a.m. to 4 p.m., Central time. Treatment includes cognitive behavior therapies, interpersonal therapy, mindfulness, medication management, family-focused strategies, health and wellness interventions, and education about mood disorders. Caregivers are required to participate in the program with their child/teen to improve understanding of their child’s illness and develop techniques to both support their child and assist with their own coping.
• Depression Improvement Across Minnesota, Offering a New Direction (DIAMOND). DIAMOND involves a primary care provider, care manager and consulting psychiatrist for Minnesota adults with depression who are seen in primary care settings, with a focus on relapse prevention. DIAMOND is currently only available for patients who have Mayo primary care providers in Rochester or Kasson, Minn.
Pain Rehabilitation Center
Mayo’s Pain Rehabilitation Center offers adult and pediatric outpatient programs for noncancer-related chronic pain to help people regain function and quality of life. These programs treat patients with a broad range of pain types, as well as those with medical and psychiatric complications. These may include chronic fatigue and nausea, fibromyalgia, cyclic vomiting, and autonomic disorders, such as postural orthostatic tachycardia syndrome (POTS). Programs include:
• Adult three-week program
• Adult two-day program
• Pediatric three-week program
Addiction Services
Since 1972, Mayo Clinic has been treating people addicted to alcohol, illegal drugs and prescription medications, using an individualized, holistic approach within a respectful environment. Multispecialty care teams include addiction psychiatrists, licensed alcohol and drug counselors, licensed clinical social workers, registered nurses and other specialists.
Learn more about Mayo’s options for addiction treatment, including the Outpatient Addiction Program, an Intensive Addiction Program and continuing care programs.
Other areas of excellence
The Department of Psychiatry and Psychology provides many other areas of excellence, such as:
• Comprehensive multidisciplinary psychiatric assessments for adults, teenagers and children
• Formal assessment of attention, concentration, memory, reasoning and learning abilities to help diagnose neuropsychological disorders such as dementia, mild cognitive impairment, traumatic brain injury, stroke, learning disabilities and attention deficits
• Clinic for attention-deficit/hyperactivity disorder (ADHD)
• Pediatric Anxiety Disorders Clinic, including treatment for panic disorder, obsessive-compulsive disorder, social phobia, generalized anxiety disorder and separation anxiety
• Behavioral Medicine Program
• Innovative memory training program called HABIT Healthy Action to Benefit Independence & Thinking®
• Telemedicine program for cognitively impaired elderly patients with behavior problems
• Rehabilitative services for people with traumatic brain injury









 Why is treatment for depression during pregnancy important?
Why is treatment for depression during pregnancy important? 

